We champion the spirit of adventure in all children!
That's why, together with our first aid expert Anna Webb*, we created a 'First aid for parents' hub to help you to treat those inevitable bumps and scrapes or anything else that might come your way!
We cover a range of common mishaps, including cuts, grazes & burns, as well as more severe accidents, such as choking or treating an unconscious child.
*Anna Webb does not endorse any medicinal brand or product.
First aid for parents - contents:
Cuts & grazes treatment
Though treating your child's first cut or cut might be upsetting, unfortunately, as your child begins to explore the world around them, the odd cut or graze is to be expected so you will soon get used to treating them. If your little one comes to you with a bump or graze, follow the next 5 steps to treat it:
Swipe images to navigate ->
Burns treatment
Though burns and scalds are less common in very young children as they tend to not be in the kitchen, cooking in the way that adults do, accidents happen. If your child gets a burn, follow the next three steps to treat it:
Swipe images to navigate ->
Burns - FAQs
.
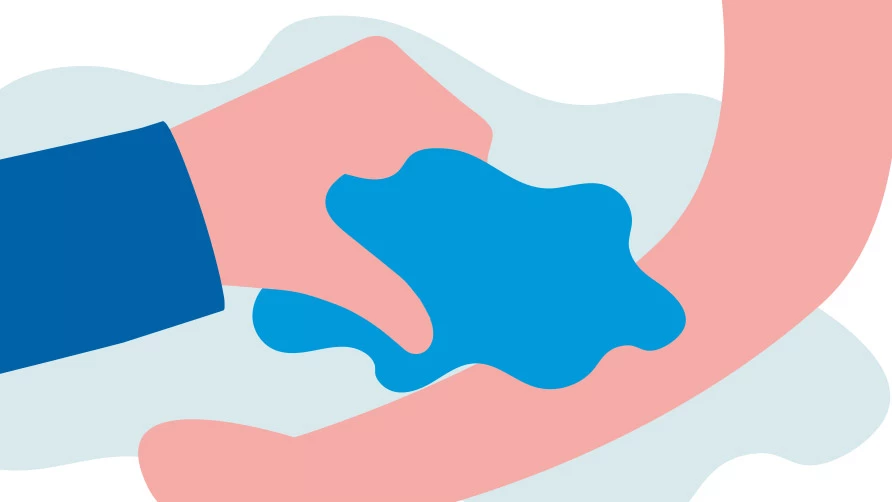
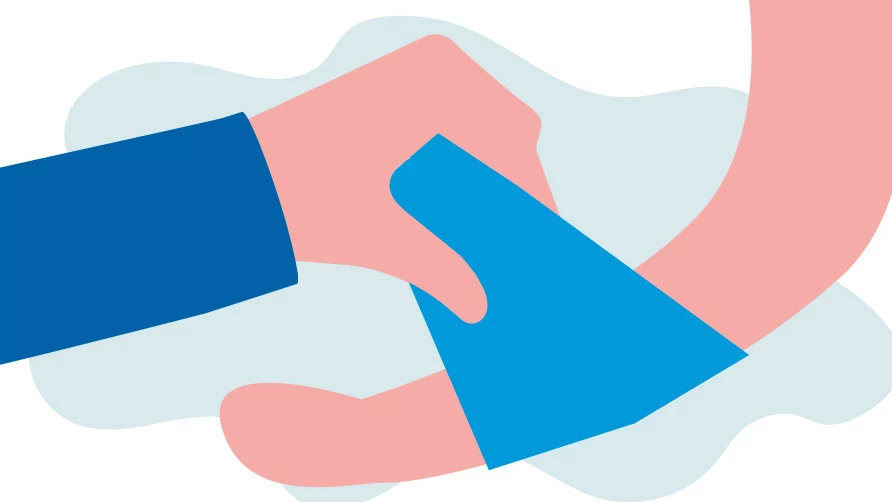
Choking in children over 1 years old
Young children will often put objects in their mouth, as it’s their natural way of exploring the world around them.
You should always keep small objects such as buttons, coins or batteries out of reach of children but sometimes, it doesn’t matter how careful you are, small enquiring hands will find something that they shouldn’t and swallow it. If you suspect that your child is choking, follow the next three steps in order:
Swipe images to navigate ->
Choking - FAQs
.
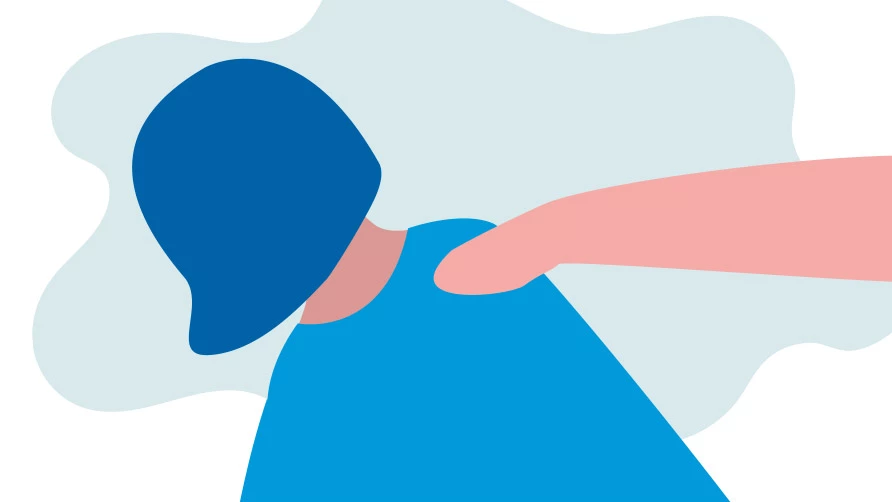
Discovery of an unconscious child who IS breathing
If a child is not moving and does not respond when you call them or gently shake their shoulders, they are unresponsive.
This can be very scary but do your best to stay calm and call 999. Whilst you wait for an ambulance, follow the next important three steps:
Swipe images to navigate ->
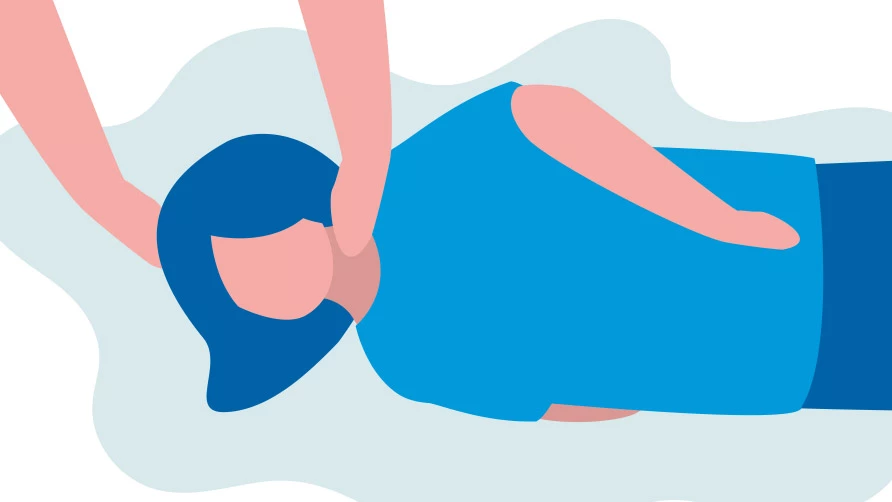
Discovery of an unconscious child who IS NOT breathing
if a child is not moving and does not respond when you call them or gently shake their shoulders, they are unresponsive.
This can be very scary but do your best to stay calm and call 999. Whilst you wait for an ambulance, follow the next important three steps:
Swipe images to navigate ->
Download & keep this guide to stay prepared
We have put all of this information into a booklet for you to refer to next time a mishap happens. Print it off and keep it within your first aid kit for ease or have a look through our Savlon Guides to learn more!
 |
Explore the Savlon range
Life should be lived to the fullest and enjoyed. And if mishaps happen along the way Savlon is always by your side.